A tooth that has been structurally damaged by decay or trauma sometimes needs to be crowned or “capped” so that it can look good and function properly again. A crown is a durable covering that is custom-made to fit over the entire tooth from the gum line up.
Getting a crown used to mean multiple office visits and weeks of waiting time, but now there is a much more convenient option—same-day crowns. Same-day crowns and other tooth restorations can be made in the dentist’s office and often in minutes using technology known as Computer-Aided Design/Computer-Aided Manufacturing (CAD/CAM).
Benefits of Same-Day Crowns
Saves you time and money
Traditional crowns require you to get temporary crowns while you wait for the permanent crown to be made. Same-day crowns eliminate the expense of the temporary crown, and the expense of the multiple appointments that traditional crowns require.
Restores function to your mouth and teeth immediately
With temporary crowns, you have to be careful how you eat so that the temporary crown doesn’t fall out. With same-day crowns, you will have full functioning of your teeth again.
Same-Day Crown Process
- Your dentist will remove any decay or debris from the affected area, and then shape the tooth or teeth so it will fit with the crown.
- With the help of a small scanning wand, your dentist will take digital pictures of your mouth that will assist in generating a 3D model of your teeth.
- The CAD/CAM software uses this 3D model to create your crown. It can even use a mirror-image twin of the other side of your mouth to create the most natural-looking crown possible.
- A block of ceramic material is chosen to match the color of your teeth, and the computer’s digital design is transmitted to a milling machine that carves the crown from the ceramic block in about five minutes.
- The crown is then bonded to your tooth.
Caring for your crown is very similar to caring for your natural teeth. As always, you need to regularly brush and floss. With crowns, it’s even more important to maintain a regular schedule of professional cleanings at the dental office. If you have a grinding habit, talk to your dentist about a mouthguard to protect your teeth and crowns.





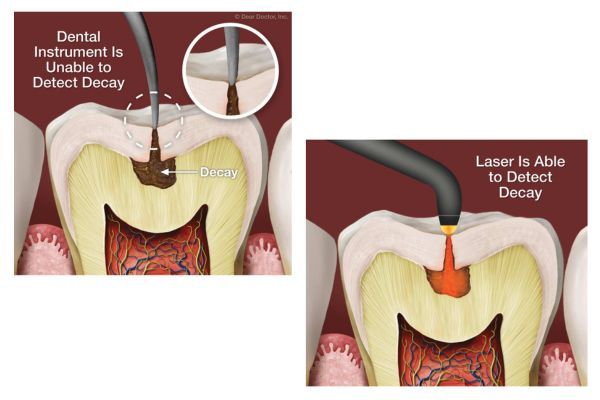



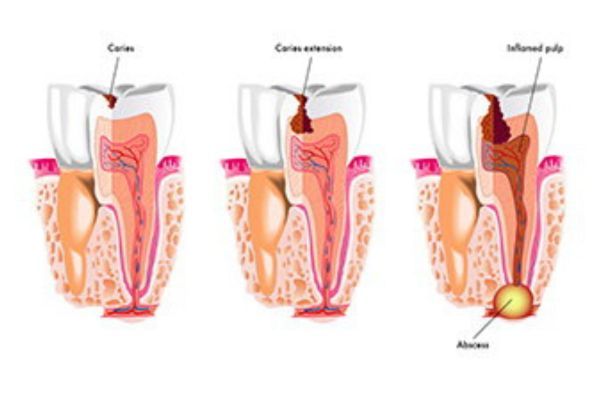
 Because tooth enamel isn’t living tissue, it can’t regenerate or grow back. Once bacteria and acids have created a deep enough cavity, only a dentist can repair it by removing the decayed area of the tooth and restoring the tooth’s structure.
Because tooth enamel isn’t living tissue, it can’t regenerate or grow back. Once bacteria and acids have created a deep enough cavity, only a dentist can repair it by removing the decayed area of the tooth and restoring the tooth’s structure.